How Evidence-based practice (EBP) can be translated as health communication or patient education materials
June 15, 2021
How to evaluate bias in meta-analysis within meta-epidemiological studies?
June 23, 2021Introduction
A case-control study is used to see if exposure is linked to a certain result (i.e., disease or condition of interest). Case-control research is always retrospective by definition since it starts with a result and then goes back to look at exposures. The investigator already knows the result of each participant when they are enrolled in their separate groups. Case-control studies are retrospective because of this, not because the investigator frequently uses previously gathered data. This article discusses statistical analysis in case-control studies.
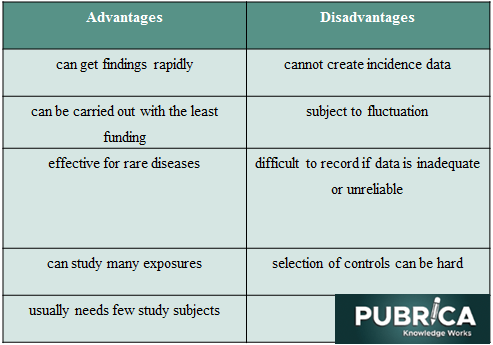
Advantages and Disadvantages of Case-Control Studies
Study Design
Participants in a case-control study are chosen for the study depending on their outcome status. As a result, some individuals have the desired outcome (referred to as cases), while others do not have the desired outcome (referred to as controls). After that, the investigator evaluates the exposure in both groups. As a result, in case-control research, the outcome must occur in at least some individuals. Thus, as shown in Figure 1, some research participants have the outcome, and others do not enrol.
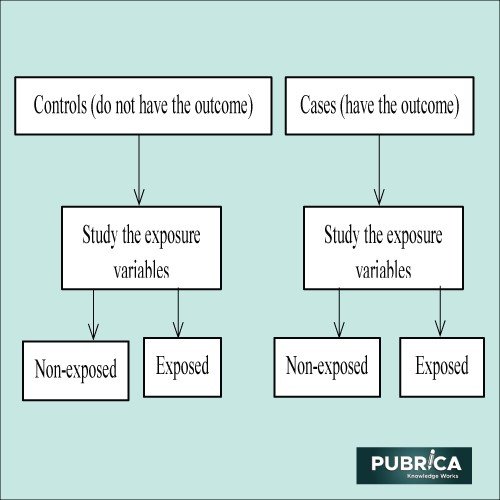
Figure 1. Example of a case-control study [1]
Selection of case
The cases should be defined as precisely as feasible by the investigator. A disease’s definition may be based on many criteria at times; hence, all aspects should be fully specified in the case definition.
Selection of a control
Controls that are comparable to the cases in a variety of ways should be chosen. The matching criteria are the parameters (e.g., age, sex, and hospitalization time) used to establish how controls and cases should be similar. For instance, it would be unfair to compare patients with elective intraocular surgery to a group of controls with traumatic corneal lacerations. Another key feature of a case-control study is that the exposure in both cases and controls should be measured equally.
Matching
Though some controls have to be similar to cases in many respects, it is possible to over-match. Over-matching might make it harder to identify enough controls. Furthermore, once a matching variable is chosen, it cannot be analyzed as a risk factor. Enrolling more than one control for each case is an effective method for increasing the power of research. However, incorporating more than two controls per instance adds little statistical value.
Data collection
Decide on the data to be gathered after precisely identifying the cases and controls; both groups must have the same data obtained in the same method. If the search for primary risk variables is not conducted objectively, the study may suffer from researcher bias, especially because the conclusion is already known. It’s crucial to try to hide the outcome from the person collecting risk factor data or interviewing patients, even if it’s not always practicable. Patients may be asked questions concerning historical issues (such as smoking history, food, usage of conventional eye medications, and so on). For some people, precisely recalling all of this information may be challenging.
Furthermore, patients who get the result (cases) are more likely to recall specifics of unfavourable experiences than controls. Recall bias is a term for this phenomenon. Any effort made by the researcher to reduce this form of bias would benefit the research.
Analysis
The frequency of each of the measured variables in each of the two groups is computed in the analysis. Case-control studies produce the odds ratio to measure the strength of the link between exposure and the outcome. An odds ratio is the ratio of exposure probabilities in the case group to the odds of response in the control group. Calculating a confidence interval for each odds ratio is critical. A confidence interval of 1.0 indicates that the link between the exposure and the result might have been discovered by chance alone and that the link is not statistically significant. Without a confidence interval, an odds ratio isn’t particularly useful. Computer programmes are typically used to do these computations. Because no measures are taken in a population-based sample, case-control studies cannot give any information regarding the incidence or prevalence of a disease.
Risk Factors and Sampling
Case-control studies can also be used to investigate risk factors for a rare disease. Cases might be obtained from hospital records. Patients who present to the hospital, on the other hand, may not be typical of the general community. The selection of an appropriate control group may provide challenges. Patients from the same hospital who do not have the result are a common source of controls. However, hospitalized patients may not always reflect the broader population; they are more likely to have health issues and access the healthcare system.
Recent research on case-control studies using statistical analyses
i) Risk factors related to multiple sclerosis in Kuwait
This matched case-control research in Kuwait looked at the relationship between several variables: family history, stressful life events, tobacco smoke exposure, vaccination history, comorbidity, and multiple sclerosis (MS) risk. To accomplish the study’s goal, a matched case-control strategy was used. Cases were recruited from Ibn Sina Hospital’s neurology clinics and the Dasman Diabetes Institute’s MS clinic. Controls were chosen from among Kuwait University’s faculty and students. A generalized questionnaire was used to collect data on socio-demographic, possibly genetic, and environmental aspects from each patient and his/her pair-matched control. Descriptive statistics were produced, including means and standard deviations for quantitative variables and frequencies for qualitative variables. Variables that were substantially (p ≤ 0.15) associated with MS status in the univariable conditional logistic regression analysis were evaluated for inclusion in the final multivariable conditional logistic regression model. In this case-control study, 112 MS patients were invited to participate, and 110 (98.2 %) agreed to participate. Therefore, 110 MS patients and 110 control participants were enlisted, and they were individually matched with cases (1:1) on age (5 years), gender, and nationality (Fig. 1). The findings revealed that having a family history of MS was significantly associated with an increased risk of developing MS. In contrast, vaccination against influenza A and B viruses provided significant protection against MS.
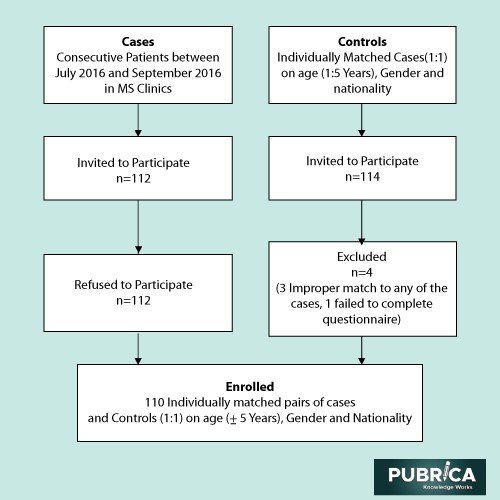
Figure 1. Flow chart on the enrollment of the MS cases and controls [1]
ii) Relation between periodontitis and COVID-19 infection
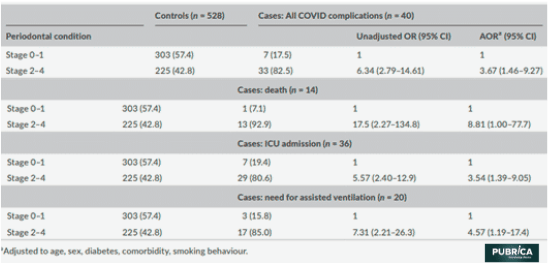
COVID-19 is linked to a higher inflammatory response, which can be deadly. Periodontitis is characterized by systemic inflammation. In Qatar, patients with COVID-19 were chosen from Hamad Medical Corporation’s (HMC) national electronic health data. Patients with COVID-19 problems (death, ICU hospitalizations, or assisted ventilation) were categorized as cases, while COVID-19 patients released without severe difficulties were categorized as controls. There was no control matching because all controls were included in the analysis. Periodontal problems were evaluated using dental radiographs from the same database. The relationships between periodontitis and COVID 19 problems were investigated using logistic regression models adjusted for demographic, medical, and behavioural variables. 258 of the 568 participants had periodontitis. Only 33 of the 310 patients with periodontitis had COVID-19 issues, whereas only 7 of the 310 patients without periodontitis had COVID-19 issues. Table 2 shows the unadjusted and adjusted odds ratios and 95 % confidence intervals for the relationship between periodontitis and COVID-19 problems. Periodontitis was shown to be substantially related to a greater risk of COVID-19 complications, such as ICU admission, the requirement for assisted breathing, and mortality, as well as higher blood levels of indicators connected to a poor COVID-19 outcome, such as D-dimer, WBC, and CRP.
Table 2. Associations between periodontal condition and COVID-19 complications [3]
iii) Menstrual, reproductive and hormonal factors and thyroid cancer
The relationships between menstrual, reproductive, and hormonal variables and thyroid cancer incidence in a population of Chinese women were investigated in this study. A 1:1 corresponding hospital-based Case-control study was conducted in 7 counties of Zhejiang Province to investigate the correlations of diabetes mellitus and other variables with thyroid cancer. Case participants were eligible if they were diagnosed with primary thyroid cancer for the first time in a hospital between July 2015 and December 2017. The patients and controls in this research were chosen at random. At enrollment, the interviewer gathered all essential information face-to-face using a customized questionnaire. Descriptive statistics were utilized to characterize the baseline characteristics of female individuals using frequency and percentage. To investigate the connections between the variables and thyroid cancer, univariate conditional logistic regression models were used. We used four multivariable conditional logistic regression models adjusted for variables to investigate the relationships between menstrual, reproductive, and hormonal variables and thyroid cancer. In all, 2937 pairs of participants took part in the case-control research. The findings revealed that a later age at first pregnancy and a longer duration of breastfeeding were substantially linked with a lower occurrence of thyroid cancer, which might shed light on the aetiology, monitoring, and prevention of thyroid cancer in Chinese women [4].
Conclusion
It’s important to note that the term “case-control study” is commonly misunderstood. A case-control study starts with a group of people exposed to something and a comparison group (control group) who have not been exposed to anything and then follows them over time to see what occurs. However, this is not a case-control study. Case-control studies are frequently seen as less valuable since they are retrospective. They can, however, be a highly effective technique of detecting a link between an exposure and a result. In addition, they are sometimes the only ethical approach to research a connection. Case-control studies can provide useful information if definitions, controls, and the possibility for bias are carefully considered.
References
[1] Setia, Maninder Singh. “Methodology Series Module 2: Case-control Studies.” Indian journal of dermatology vol. 61,2 (2016): 146-51. doi:10.4103/0019-5154.177773
[2] El-Muzaini, H., Akhtar, S. & Alroughani, R. A matched case-control study of risk factors associated with multiple sclerosis in Kuwait. BMC Neurol 20, 64 (2020). https://doi.org/10.1186/s.
[3] Marouf, Nadya, Wenji Cai, Khalid N. Said, Hanin Daas, Hanan Diab, Venkateswara Rao Chinta, Ali Ait Hssain, Belinda Nicolau, Mariano Sanz, and Faleh Tamimi. “Association between periodontitis and severity of COVID‐19 infection: A case–control study.” Journal of clinical periodontology 48, no. 4 (2021): 483-491.
[4] Wang, Meng, Wei-Wei Gong, Qing-Fang He, Ru-Ying Hu, and Min Yu. “Menstrual, reproductive and hormonal factors and thyroid cancer: a hospital-based case-control study in China.” BMC Women’s Health 21, no. 1 (2021): 1-8.