Health economics in clinical trials
April 8, 2021
How EBP Can Be Used For Technology Development
April 15, 2021Brief:
Leaning to the side of science, everyone in the modern world wants to stick with the based and the proven evidence. More efforts by the researchers have been put into the research and experiments to vouch for the new practices and discoveries. Evidence-Based Practice (EBP) is one such methodology that helps interlinking the various scientifically proven for the welfare of an individual or the society.
Introduction
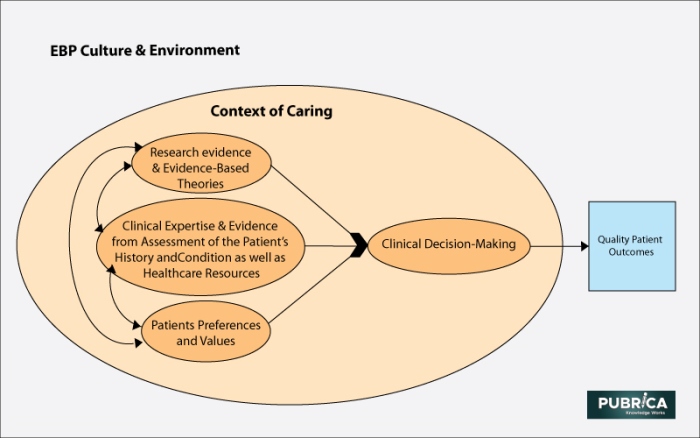
Evidence Based Practice (EBP) enables the proper delivery of knowledge and updates in the health field. EBP can be defined as the integrator that interlinks – Clinical expertise, research evidence, and data from the practice content and also provides clinical literature review. However, the purpose of EBP is to assist in clinical decision-making for better treatment of the patients.
The history of EBP starts in 1970. Before the EBP, the health professionals mostly tended to rely on other experienced health professionals. Though the required information is easily accessible and based, there can be mistakes or prone to incorrect leads pertaining to the health professionals’ age and memory. Sometimes, the clinical experience would even be biased based upon the varying past of the professionals.
Regular steps in EBP
Firstly the ‘need’ is assumed by considering the situations. The various resources that are proven with scientific evidence are acquired. Those resources must justify their answers with strong research work in the background.
Lastly, the collected data are analyzed for relevance to the situation that the health professional undergoes.
After all, with the data collected, situations are handled appropriately. Furthermore, their results are also recorded for future studies.
Feature of EBP
Unlike the regular guidelines, instructions, recommendations, etc., EBP ensures better clinical practice. EBP sounds like the randomized controlled trials where the treatments are investigated. All the information required by the health professionals can be collected without much strain.
Necessity of EBP
Not every patients’ conditions would be easily treatable. Depending upon the scenarios the treatments are altered to ensure the stability of the patients. Therefore, it is always important to understand the scientific advantages of proven scientific evidence.
Health professionals thought process helps the most in acquiring the knowledge from the proven scientific evidences. Critical thinking on the situations by introspecting – why this happens? how does this happen? what could be the way to get rid of this? In the end, with the situation pushing them, they start collecting the information from various sources and start relating to the situation.
For example, we shall consider a situation where the patient is undergoing bed rest after surviving a heart attack. Bed rest after the heart attack is the recommended one based upon the previous knowledge of the clinical experts citing the reason that the heart requires more rest and must be kept away from emotional imbalance. But the randomized controlled trials show that bed rest could make thromboembolism which is a dangerous condition that could block the blood flow via blood vessels.
Quality of the research publication
There are plenty of sources available these days and the most exceptional one is the Internet where we collect more data such articles, review chapters, etc. But the quality of the content containing the relevant information is the most important thing to be considered before proceeding to utilize the data. The collected data must ensure validity, compliance, aftermath effects.
Advantages & Disadvantages of EBP
Evidence-Based Practices possess their advantages. EBP ensures the quality of information that is provided to the professionals. The professionals can provide the appropriate treatment and balance the other critical conditions of the patients. The decisions made on the evidence-based medicine can be believed with more confidence.
Though EBP promises to be the better reliable method while comparing with others, there also exist certain disadvantages within it. EBP needs more accurate information and proven evidence which may consume more time. Considering the unexpected situations with patients, a professional may not start the research work to tackle the issues immediately.
Criticisms of EBP
Though the qualitative research is the most welcomed type of research. EBP is criticized for relying more upon quantitative research. Many professionals around the globe question the definitions of the term – Evidence in Evidence-Based Practice. They argue that, based upon the perception towards the problem, the evidence can be both correct as well as incorrect. Furthermore, clinical experience is also given an equal part in creating the evidence, thus questioning the certainty and biasness.
Conclusion
Creating the evidence and connecting them to the appropriate situations is not a one-day matter. There involved a lot of difficulties in experimentation, collection of data from various sources, and bringing them to the right situation at right time. Apart from all, it keeps on updating itself based on the new situations that arise after new cases.
References
- Djulbegovic, B., & Guyatt, G. (2020). Evidence-based medicine in times of crisis. Journal of clinical epidemiology, 126, 164-166.
- B Jensen, I., Björk Brämberg, E., Wåhlin, C., Björklund, C., Hermansson, U., Lohela Karlson, M., Schäfer Elinder, L., Munck Af Rosenschöld, P., Nevala, T., Carter, N., Mellblom, B., & Kwak, L. (2020). Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach. International journal of environmental research and public health, 17(15), 5283. https://doi.org/10.3390/ijerph17155283.
- Spence, J. D. (2020). The need for clinical judgement in the application of evidence-based medicine. BMJ evidence-based medicine, 25(5), 172-177.
- Hasanpoor, E., Janati, A., Arab-Zozani, M., & Haghgoshayie, E. (2018). Using the evidence-based medicine and evidence-based management to minimize overuse and maximize quality in healthcare: a hybrid perspective. BMJ Evidence-Based Medicine, bmjebm–2018–110957. doi:10.1136/bmjebm-2018-110957
- Anjum, R. L., Copeland, S., & Rocca, E. (2020). Medical scientists and philosophers worldwide appeal to EBM to expand the notion of ‘evidence’. BMJ evidence-based medicine, 25(1), 6-8.