- Services
- Discovery & Intelligence Services
- Publication Support Services
- Sample Work
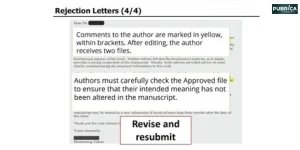
Publication Support Service
- Editing & Translation
Editing and Translation Services
- Sample Work

Editing and Translation Service
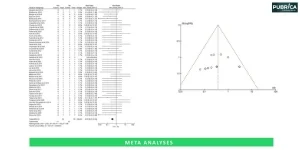
- Research Services
- Sample Work
Research Services
- Physician Writing
- Sample Work

Physician Writing Service
- Statistical Analyses
- Sample Work
Statistical Analyses
- Data Collection
- AI and ML Services
- Research Impact
- Sample Work
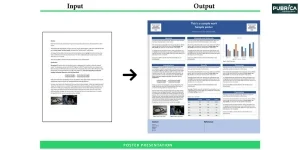
Research Impact
- Medical & Scientific Communication
- Medico Legal Services
- Educational Content
- Industries
- Subjects
- About Us
- Academy
- Insights
- Get in Touch
- Services
- Discovery & Intelligence Services
- Publication Support Services
- Sample Work
Publication Support Service
- Editing & Translation
Editing and Translation Services
- Sample Work

Editing and Translation Service
- Research Services
- Sample Work
Research Services
- Physician Writing
- Sample Work

Physician Writing Service
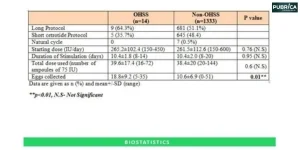
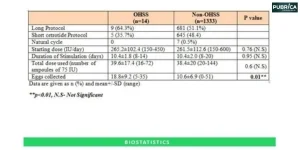
- Statistical Analyses
- Sample Work
Statistical Analyses
- Data Collection
- AI and ML Services
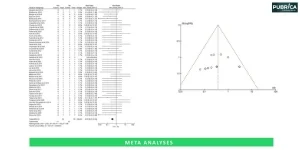
- Research Impact
- Sample Work
Research Impact
- Medical & Scientific Communication
- Medico Legal Services
- Educational Content
- Industries
- Subjects
- About Us
- Academy
- Insights
- Get in Touch
As of April 2025, ongoing legislative efforts to restructure prior authorization in Medicare have been accelerating, with bipartisan sponsorship and enthusiasm from large medical organizations. The Reducing Medically Unnecessary Delays in Care Act of 2025 (H.R. 2433), introduced on April 4, 2025, seeks to make certain that treatment decisions can only be reviewed by specialty board-certified physicians, thus dispelling fears that the misuse of prior authorization reduces patient care.
- Home
- Insights
- News
- Legislative Efforts to Reform Prior Authorization in Medicare
Legislative Efforts to Reform Prior Authorization in Medicare
Best Practices for Writing AI-Assisted Manuscripts


Dr.Nanci | Research design and Mixed Methods Research.
30 Jan, 2025

Dr.Nanci | Research design and Mixed Methods Research. 30 Jan, 2025
April 2025 | Source: American Medical Association
As of April 2025, ongoing legislative efforts to restructure prior authorization in Medicare have been accelerating, with bipartisan sponsorship and enthusiasm from large medical organizations. The Reducing Medically Unnecessary Delays in Care Act of 2025 (H.R. 2433), introduced on April 4, 2025, seeks to make certain that treatment decisions can only be reviewed by specialty board-certified physicians, thus dispelling fears that the misuse of prior authorization reduces patient care.
Legislative Developments
- The Reducing Medically Unnecessary Delays in Care Act of 2025 (H.R. 2433) was introduced by Rep. Mark Green, M.D., to tackle prior authorization requirements in Medicare and Medicare Advantage and fix prior authorization to prescription drug plans under Medicare.
- The bill provides that prior authorization decisions should be made by board-certified physicians in the relevant specialty, and prior authorization restrictions in the plans should be based on medical necessity and written clinical criteria. The legislation also includes transparency obligations for Medicare, Medicare Advantage, and Medicare Part D plans.
- At the same time, the Improving Seniors’ Timely Access to Care Act has gained considerable bipartisan support of more than 220 cosponsors in the House and 54 in the Senate.
- The bill attempts to constrain the previous authorization and notice process in Medicare Advantage by taking electronic capabilities, keeping heirs safe while transitioning plans, having formalized procedures, and ensuring opinions are timely and reviewed by qualified medical staff.
Administrative Actions
The Centers for Medicare & Medicaid Services (CMS) has finalized regulations to improve prior authorization processes, taking effect in 2026 and 2027. These rules will electronically streamline prior authorization for Medicare Advantage, Medicaid, and CHIP programs. The rule will also require insurers to give a specific reason for denials and publicly report information about their approval and denial rates.
Advocacy and Support
- The AMA (American Medical Association) supports prior authorization reform because of its administrative burden and the risk it poses to patient care. It advocates legislation that increases the accountability, transparency of insurers, and states that legal action should be taken when harm is done to patients because of prior authorization delays.
- The AMA also calls for insurers to provide clarity and transparency when denying coverage. These efforts are intended to help streamline care and protect patient health.
- The American College of Physicians (ACP) and other organizations have called on Congress to reform the prior authorization process, stressing its importance to patient protection and the administrative burden on the health care workforce.
What This Means for Researchers
The introduction of H.R. 2433 has serious ramifications for researchers studying health policy, directors of clinical trials, and analysts of healthcare systems. This reform promises transparency and efficiency in the way that treatments can be approved in Medicare and Medicare Advantage. Increased treatment approval times will provide:
- Timely Data Access to do real-world evidence studies.
- Better enrolment in Trials, especially for older adults.
- New Policy Research Opportunities related to health systems and access to real-world evidence.
How Pubrica Supports These Changes
At Pubrica, we understand that prior authorization has been a longstanding barrier not just for patient care, but also for the continuum of research. As a top provider of research consulting and regulatory writing services, Pubrica supports these legislative reforms in the following ways:
- Incorporating Regulatory Updates into study protocols.
- Creating Trials that are properly designed with reduced authorization delays.
- Completing Health Economics and Outcomes Research (HEOR) Analyses of policy implications and health economic value.
Pubrica’s Viewpoint
Pubrica endorses the bipartisan effort behind H.R. 2433 as a critical step toward evidence-based healthcare delivery. We support:
- Patient Care + Research: Timeliness provides proper treatment and reliable data.
- Specialist Review: Decisions are only made by Board-certified physicians, guaranteeing that they are clinically appropriate and ethical.
- Less Delay, Better Data: Faster processes yield newer data, which tends to be cleaner (meaning less costly and better for research use).
Conclusion
The momentum toward reforming prior authorization in Medicare is moving forward with legislative proposals and administrative actions designed to eliminate delays to care, improve transparency, and ease provider burden. It will be vital that medical organizations continue their advocacy and that the bipartisan support we’ve seen in Congress continues as we work to enact meaningful reforms and enhance patient access to the medical care they need.
Partner with Pubrica to navigate regulatory shifts and accelerate your research outcomes. Leverage our expertise to integrate policy reforms into compliant, patient-centric study designs.

