- Services
- Discovery & Intelligence Services
- Publication Support Services
- Sample Work
Publication Support Service
- Editing & Translation
Editing and Translation Services
- Sample Work

Editing and Translation Service
- Research Services
- Sample Work
Research Services
- Physician Writing
- Sample Work

Physician Writing Service
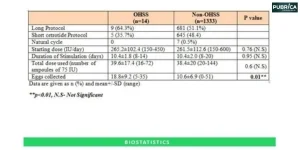
- Statistical Analyses
- Sample Work
Statistical Analyses
- Data Collection
- AI and ML Services
- Research Impact
- Sample Work
Research Impact
- Medical & Scientific Communication
- Medico Legal Services
- Educational Content
- Industries
- Subjects
- About Us
- Academy
- Insights
- Get in Touch
- Services
- Discovery & Intelligence Services
- Publication Support Services
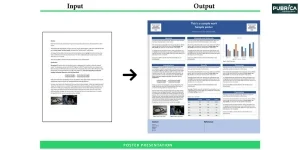
- Sample Work
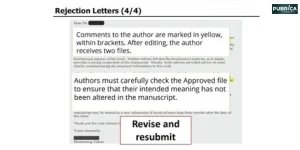
Publication Support Service
- Editing & Translation
Editing and Translation Services
- Sample Work

Editing and Translation Service
- Research Services
- Sample Work
Research Services
- Physician Writing
- Sample Work

Physician Writing Service
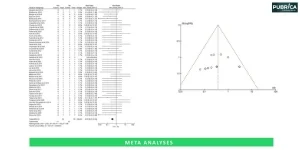
- Statistical Analyses
- Sample Work
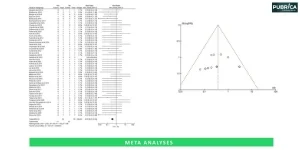
Statistical Analyses
- Data Collection
- AI and ML Services
- Research Impact
- Sample Work
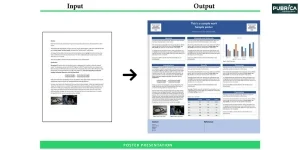
Research Impact
- Medical & Scientific Communication
- Medico Legal Services
- Educational Content
- Industries
- Subjects
- About Us
- Academy
- Insights
- Get in Touch
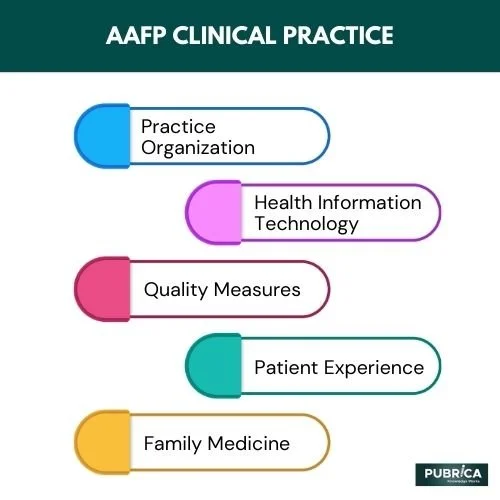
AAFP Clinical Practice Guideline Manual
The American Academy of Family Physicians (AAFP) creates evidence-based clinical practice guidelines (CPGs) that serve as a foundation for clinical choices and best practices. Clinical practice guidelines are statements that provide suggestions to improve patient care. They are based on thoroughly examining the data and assessing the benefits and drawbacks of alternative care alternatives. To enhance patient outcomes, CPGs should adhere to a robust, transparent framework for translating the best evidence into clinical practice. Furthermore, evidence-based CPGs are an essential component of patient-centred treatment.
- Clinical practice guidelines should be established using a rigorous evidence-based approach, with the level of evidence for each guideline specified explicitly.
- Clinical performance metrics may be established from clinical practice standards and utilized in quality improvement programs if they are realistic, quantifiable, and attainable. When these performance indicators are included in public reporting, accountability, or pay-for-performance initiatives, the strength of the evidence and scale of the benefit should be adequate to justify the implementation burden.
- In the clinical context, implementation of clinical practice recommendations should be prioritized to those with the most robust supporting evidence and the most significant impact on morbidity and mortality in the patient group.
- There should be more research on properly adopting clinical practice guidelines and the effects of using them as quality measurements(1).
Development of Evidence-based Clinical Practice Guidelines (CPGs)
Clinical practice guidelines include suggestions to improve patient care based on a systematic review examination of evidence and an assessment of the advantages and hazards of alternative care alternatives. For example, instead of prescribing a one-size-fits-all strategy for patient care, clinical practice guidelines include evaluating the quality of the appropriate scientific literature and assessing the potential benefits and hazards of a particular treatment. Depending on this information, healthcare practitioners may choose the optimal care for a specific patient based on their preferences.
Collaboration on CPG Development with External Organizations (CMSS P 9)
The AAFP supports the creation of unambiguous patient-centred clinical practice recommendations that emphasize what should be done for patients rather than who should do it. When clinical practice guidelines address who should provide care, management, consultation, or referral, suggestions should stress particular relevant abilities rather than a clinician’s speciality classification. For example, when specific requirements are satisfied, the AAFP may collaborate with other medical organizations to formulate clinical practice guidelines (also known as practice parameters or clinical policies).
Identification of a CPG Clinical Topic
- Importance in family medicine
- There are no current evidence-based recommendations on the issue that are appropriate for use by family doctors.
- This guidance will help AAFP’s Strategic Objectives and Strategies.
- A systematic evidence report is available, and the issue may be submitted to the Agency for Healthcare Research and Quality (AHRQ), or funding for the preparation of an evidence review is available.
CPG Clinical Topic Systematic Evidence Review (IOM Standard 4)
In most situations, the AAFP works with the Agency for Healthcare Research and Quality (AHRQ) to independently assess the evidence based on the CPG’s core issues.
CPG Panel Development (IOM Standards 3; CMSS-P 4)
The Guideline Development Group is formed by staff in collaboration with the chairpersons of SCRP and CHPS.
Potential Conflict of Interest (COI) Policy and Process (IOM Standard 2, CMSS-P 3, CMSS-C 7.5-7.8)
A possible source of bias in creating CPGs is a conflict of interest (COI). A conflict of interest (COI) is described as a set of circumstances in which professional judgment on a primary claim (guideline recommendations) is inappropriately impacted by a secondary interest (financial or intellectual interests)
Clinical Practice Guideline Panel Collaboration
AAFP staff members will create a timetable for the guideline’s development in consultation with the GDG chair. This timeline will be provided to GDG members during the GDG’s first meeting. Though this timeline was created to adhere to it, it is acknowledged that situations throughout the development process may change it. As a result, this is a live document that should be updated during the guideline process.
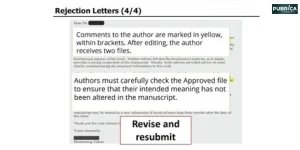
Report on Review of Published Evidence (IOM Standard 4)
If there have been more than 12 months from the publication of an AHRQ evidence review and the creation of the recommendation, the systematic review will be updated. The GDG and AAFP personnel will collaborate with the AAFP librarian to complete the revised assessment. The librarian will employ the same search parameters as the AHRQ systematic review. Inclusion and exclusion criteria will be established in advance to identify which papers will be examined for quality. In addition, AAFP staff members review the updated search results to find documents relevant to the systematic review.
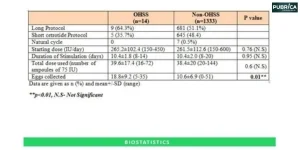
Evidence Evaluation and Recommendation Strength (CMSS-P 6; IOM Standards 5 and 6)
A systematic review starts with gathering evidence and assessing its quality. The strength of the suggestions in the guideline should be connected to the quality of the evidence. The AAFP utilizes a specific approach to evaluate the research quality and gives strength to each recommendation, which is consistent with the IOM guidelines for systematic reviews.
Writing the Guideline
All AAFP guidelines include the objective, reasoning, and scope. This includes, but is not limited to, the suitable users of the guideline, scenarios in which the guideline should be applied, and patient groups for which the guideline is appropriate.
Give yourself the academic edge today
Each order includes
- On-time delivery or your money back
- A fully qualified writer in your subject
- In-depth proofreading by our Quality Control Team
- 100% confidentiality, the work is never re-sold or published
- Standard 7-day amendment period
- A paper written to the standard ordered
- A detailed plagiarism report
- A comprehensive quality report