Microcirculation Under Inflammation: Industry Perspectives and Market Trends
Introduction
Microcirculation describes the portion of the circulation system that deals with the smallest units of blood vessels. It is, concerned with the delivery of nutrients and oxygen to tissues and the removal of waste. The healthiness of the microvascular network is of paramount importance to the maintenance of tissue homeostasis and good health in general [1]. Its optimal blood flow and cellular well-being are essentially managed through a fine balance between vasodilation and vasoconstriction, and its dysregulation can lead to pathological conditions. Inflammation is a biological response aimed at restoring the tissue integrity post injury or infection, but chronic inflammation leads to microcirculation damage due to damage to endothelial cells, promotion of vascular permeability, leukocyte adhesion, and thrombosis [1]. It leads to increased permeability and edema that causes tissue hypoxia and long recovery time in the affected area. This article explores the latest therapeutic technologies, diagnostic equipment, and pharmaceutical inventions for counteraction against inflammation-induced microcirculation, providing industry insights and market trends.
Impact of Inflammation on Microcirculation
Pathophysiology
Inflammatory responses lead to endothelial activation, causing leukocyte adhesion and vascular permeability. These processes impair perfusion and nutrient exchange in affected tissues, thereby perpetuating inflammation [3]. This causes a chain reaction with vasodilation, activation of leukocytes, and often thrombosis that decreases the efficiency of microcirculation even further.
Clinical Manifestations
Common results include tissue hypoxia, edema, and even organ dysfunction. For instance, chronic inflammation has been associated with many cardiovascular diseases and ICU-acquired weakness, whereby systemic inflammation is believed to affect several organs [4]. In severe cases, inflammatory disruption can progress to other serious conditions like sepsis-induced microcirculatory dysfunction, particularly irregular patterns and vessel congestion, leading to tissue ischemia [7]. These symptoms emphasize the importance of treating microvascular inflammation to improve patient outcomes.
Long-term Effects
Chronic inflammation, particularly in diabetes and hypertension, can cause fibrotic tissue changes, prolonged edema, and sustained hypoxia, leading to extensive damage through microcirculation [5]. Prolonged inflammation in microvasculature may cause chronic conditions such as vascular sclerosis, poor wound healing, and organ dysfunction. For instance, chronic inflammation can cause conditions like atherosclerosis that would directly affect the structural integrity of blood vessels and reduce tissue perfusion (Dong et al., 2022). The prevention and treatment of these long-term complications requires a combination of preventive and therapeutic approaches and microvascular protection.
Industry Perspectives on Microcirculation in Inflammatory Conditions
Pharmaceutical Innovations
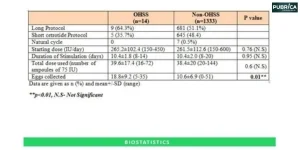
The pharmaceutical industry has developed numerous drugs related to specific inflammation-mediated microcirculatory dysfunction. Anti-inflammatory drugs like corticosteroids are largely used, but newer biologics that target cytokines like TNF-α and IL-1β can help reduce endothelial damage and improve flow in the microvasculature [6]. Similarly, agents PCSK9 inhibitors are producing good results in enhancing the function of microcirculation in patients with coronary conditions post-PCI, according to PMC, 2023 [1].
Technological Advances
Inflammation often interrupts microcirculation and generally causes tissue hypoxia and edema. This can lead to more complicated problems, such as microcirculatory dysfunction caused by sepsis with disorders in unidirectional blood flow and vessel congestion, and hence tissue ischemia [7]. Thus, treating microvascular inflammation proves of importance to the recovery of such patients. Further, new developments in diagnostics of microcirculation using high-resolution imaging and biomarkers at the molecular level are emerging as valuable tools to detect inflammation-related problems very early and monitor their courses [8] [5]. For example, direct assessment of capillary density and blood flow devices are currently being used in clinical trials and ICU settings.
Therapeutic Approaches
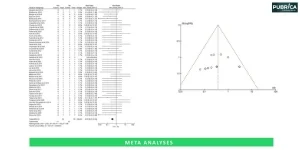
Beyond pharmaceuticals, endothelial repair and function therapies are increasing in the limelight. To this extent, an angiogenic therapy designed to induce the growth of new vessels in damaged tissue is a novel approach to restoring microvascular integrity. Other promising evidence includes low-level laser therapy that minimizes inflammation and enhances local blood flow, providing a distinct therapeutic approach to managing chronic microcirculatory conditions [7]. Anti-inflammatory therapies with monoclonal antibodies and blockers of cytokines are now being added to therapy to preserve microcirculatory function in diseases like rheumatoid arthritis or sepsis [10]. Nanotechnology is the latest technology used to achieve targeted drug delivery to suppress systemic inflammation, thus allowing for localized and more efficient intervention. Moreover, these therapies are found to be effective in maintaining the endothelium in healthy conditions in cases of inflammatory stress [9].
Conclusion
In conclusion, interplays involving inflammation as well as that with the microcirculatory aspect can pave the way for developing effective treatment plans. Chronic inflammation results in severe microvascular dysfunction that ultimately affects tissue health and serves as a component for related diseases. The drug and technology advances in the sector have heralded new openings for early diagnosis and targeted treatment that continue to enhance patient outcomes. Research development is significant as innovative approaches are incorporated in the microcirculatory health challenges posed by inflammation, improving the clinic management of related conditions.
References
- Ji, J., Wei, X., Chen, W., Wan, D., Han, W. and Liu, H. (2023) Effects of early PCSK9 inhibitor application on inflammation levels and microcirculatory function after PCI in patients with NSTE-ACS. American Journal of Translational Research, 15(5), p.3586.
- Goertz, O., Ring, A., Buschhaus, B., Hirsch, T., Daigeler, A., Steinstraesser, L., Steinau, H.U. and Langer, S., (2011) Influence of anti-inflammatory and vasoactive drugs on microcirculation and angiogenesis after burn in mice. Burns, 37(4), pp.656-664.
- Schindler, T.H. and Bhandiwad, A. (2023) Coronary Microvascular Dysfunction: Linking Inflammation and Cardiac Dysfunction?. Basic to Translational Science, 8(2), pp.152-154.
- Mendelson, A.A., Erickson, D. and Villar, R., 2023. The role of the microcirculation and integrative cardiovascular physiology in the pathogenesis of ICU-acquired weakness. Frontiers in Physiology, 14, p.1170429.
- Guven, G., Hilty, M.P. and Ince, C. (2020) Microcirculation: physiology, pathophysiology, and clinical application. Blood purification, 49(1-2), pp.143-150.
- Wang, Y., Wang, B., Ling, H., Li, Y., Fu, S., Xu, M., Li, B., Liu, X., Wang, Q., Li, A. and Zhang, X., 2024. Navigating the Landscape of Coronary Microvascular Research: Trends, Triumphs, and Challenges Ahead. Reviews in Cardiovascular Medicine, 25(8), p.288.
- Fan, D. and Wu, R., 2024. Mechanisms of the septic heart: From inflammatory response to myocardial edema. Journal of Molecular and Cellular Cardiology.
- Wang, W., Xu, D., Ding, J., Zhang, W., Fan, J. and Wang, D., 2023. Nanocarrier Based Targeting of Vascular Cell Adhesion Molecule-1 for Diagnosis and Treatment of Atherosclerosis: Current Status and Future Perspectives. Journal of Biomedical Nanotechnology, 19(7), pp.1105-1127.
- Dong, M., Shi, Y., Yang, J., Zhou, Q., Lian, Y., Wang, D., Ma, T., Zhang, Y., Mi, Y., Gu, X. and Fan, R., 2020. Prognostic and clinicopathological significance of systemic immune-inflammation index in colorectal cancer: a meta-analysis. Therapeutic advances in medical oncology, 12, p.1758835920937425.
- Ye, X., Wang, S., Wu, Q., Lv, Y., Lv, Q., Li, J., Li, L. and Yang, Y., 2023. Effects of PCSK9 inhibitors on coronary microcirculation, inflammation and cardiac function in patients with CHD after PCI: a protocol for systematic review and meta-analysis. BMJ open, 13(9), p.e074067.