A Case Report of Type 1 Diabetes During the COVID-19 Vaccine
October 21, 2023
How Randomized Controlled Trials are Used in Meta-Analysis
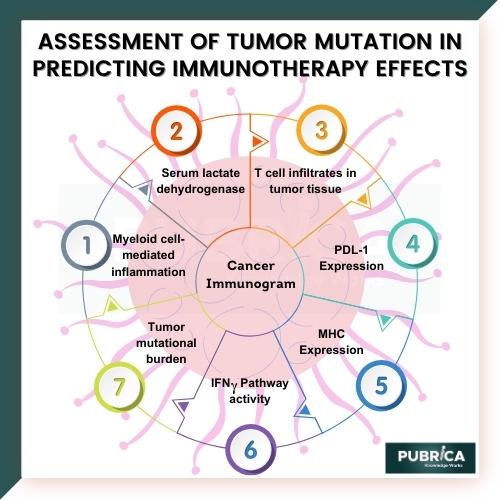
November 8, 2023Immunotherapy has emerged as an innovative approach to cancer treatment, but its effectiveness varies widely among patients. Tumor mutation burden (TMB) has been proposed as a potential predictive biomarker for immunotherapy response. This study aims to conduct a meta-analysis and bioinformatics assessment of TMB’s role in predicting immunotherapy effects across various cancer types. Through a comprehensive review of existing literature and the integration of large-scale genomic datasets, we seek to elucidate the relationship between TMB and immunotherapy outcomes. Our findings may contribute to the refinement of patient selection criteria for Immunotherapy and the development of personalized treatment strategies.
Introduction
Cancer is a prominent cause of mortality and a major impediment to extending life expectancy, and new cases continue to climb in practically every country throughout the world. Surgery, radiation, chemotherapy, and targeted therapy have long been recognized as the primary cancer treatment approaches. The development of Immunotherapy has transformed cancer treatment. With the use of immune checkpoint inhibitors (ICIs), several significant improvements in cancer treatment have been made.
Immunotherapy, which harnesses the immune system’s ability to target and destroy cancer cells, has revolutionized cancer treatment. However, its success in achieving durable responses varies among patients, emphasizing the need for reliable predictive biomarkers. Tumour mutation burden (TMB), the total number of mutations within a tumour genome, has gained attention as a potential indicator of immunotherapy response. TMB’s role in predicting immunotherapy effects, though promising, remains a subject of ongoing investigation.
Methods:
- Literature Review: We will systematically review existing studies and clinical trials that have investigated the association between TMB and immunotherapy response. Studies meeting predefined inclusion criteria will be considered for the meta-analysis.
- Data Extraction: Data on TMB levels, immunotherapy outcomes, and other relevant parameters will be extracted from selected studies.
- Meta-analysis: Statistical analysis will be performed to assess the overall effect size of TMB on immunotherapy response. Subgroup analyses will be conducted based on cancer type and immunotherapy approach.
- Bioinformatics Assessment: We will analyze large-scale genomic datasets to explore the molecular mechanisms underlying the relationship between TMB and immunotherapy response. This will include investigating the tumour microenvironment, immune cell infiltration, and neoantigen load.
- Integration of Findings: The meta-analysis results and bioinformatics findings will be integrated to provide a comprehensive assessment of TMB’s predictive value in the context of Immunotherapy.
Selection criteria
The study uses the following inclusion criteria:
- All the patients were diagnosed with cancer, and tumour tissue-based TMB was detected.
- At least one ORR, DCB, OS and PFS data could be available.
- The sample size was greater than 20.
- Studies on nonsynonymous mutations were also included due to the consistency of the measurement principle.
- Patients treated with ICIs monotherapy. On the other hand, studies that met any of the following.
Criteria were excluded:
- TMB is detected from circulating tumour DNA or blood.
- The definition of high TMB and low TMB was not clear, nor was TMB obtained by a machine learning model.
- The sample size was less than 20, or the main observed events cannot be obtained.
- Patients who had not been treated with ICIs or had received treatment other than ICIs at the same time.
- Non-human studies, conference abstracts, reviews, meta-analyses, comments or letters.
Data extraction and quality assessment
Two independent researchers (CJL, YX) assessed article titles and abstracts, and studies that met the selection criteria were retrieved for full-text evaluation. The literature quality evaluation was also done during data extraction. A third investigator (CSY) helped to address several discrepancies. The first author, publication year, country of study, study type, cancer type, cancer stage, immunotherapy drug, target point of the medicine, TMB detection method, TMB cut-off value, number of patients with high/low TMB, and corresponding data of DCB, ORR, OS, and PFS were extracted into an Excel spreadsheet.
Bioinformatics analysis
We obtained data on simple nucleotide variation (SNV) from the TCGA database (portal.gdc.cancer.gov/). The workflow type was MuTect2 Variant Aggregation and Masking, and the data format was maf. The TMB of each sample was then calculated using the Maftools R program. The Kaplan-Meier analysis for overall survival was then performed using R software and the Log-Rank to test the TMB of 33 tumours, with the cut-off level set at 70%. The K-M analysis findings are displayed as a forest plot.
Statistical analysis
Stata 16.0 software (Stata Corporation, College Station, Texas, USA) was used for all meta-analyses, and ORR, DCB, OS, and PFS were compared between high TMB and low TMB groups using meta-analysis. For DCB and ORR, RR > 1 indicated that the high TMB group outperformed the low TMB group. For combined HR and 95% CI OS/PFS data, HR > 1 shows that the high TMB group has a worse survival rate than the low TMB group. When I2 was larger than 50%, the random-effect model was employed, and when I2 was less than 50%, the fixed-effect model was utilized. Furthermore, we conducted a subgroup analysis of OS and PFS for various tumour kinds, locations, and TMB detection techniques.
Discussion
The results of this study are expected to shed light on the utility of TMB as a predictive biomarker for immunotherapy effects in cancer treatment. Understanding the molecular mechanisms and factors influencing TMB’s impact on immunotherapy response will contribute to the development of personalized treatment strategies and may help refine patient selection criteria for Immunotherapy.
- To know more about biostatistics services, check our study guide on the significance of clinical research in biostatistics.
Conclusion
The integration of meta-analysis and bioinformatics approaches will provide valuable insights into the role of TMB in predicting immunotherapy effects. This research has the potential to advance the field of cancer immunotherapy and improve patient outcomes by guiding treatment decisions based on tumour mutation burden.Although further studies are needed to establish the optimal approach to the application of TMB in practice, these results support that TMB is a promising predictive biomarker that can predict clinical bioinformatics response and prognostic outcome of Immunotherapy. Our findings thus lend support to high TMB as a therapeutic biomarker that can improve the management of cancer immunotherapy.
Check our Examples to get an understanding of our adaptability across biostatistics topics and subject domains.
References
- Sasaki, Hironobu, et al. “Newly developed type 1 diabetes after coronavirus disease 2019 vaccination: A case report.” Journal of Diabetes Investigation 13.6 (2022): 1105-1108.
- Yano, Masahiro, et al. “New-onset type 1 diabetes after COVID-19 mRNA vaccination.” Internal Medicine 61.8 (2022): 1197-1200.
- Sakurai, Kanako, et al. “Type 1 diabetes mellitus following COVID‐19 RNA‐based vaccine.” Journal of diabetes investigation 13.7 (2022): 1290-1292.