A systematic review of machine learning methods for predicting cardiovascular disease
October 12, 2023
Meta-analysis and Bioinformatics Assessment of Tumour Mutation in Predicting Immunotherapy Effects
October 26, 2023The coronavirus disease 2019 (COVID-19) vaccination has been linked to the development or worsening of diabetes. A case report of a 73-year-old Japanese lady who was given two doses of the Moderna COVID-19 vaccine, which resulted in worsening glycemic control and the emergence of type 1 diabetes. The patient exhibited a disease-susceptible human leukocyte antigen haplotype and was highly immunoreactive. The duration between immunization and the onset of type 1 diabetes was greater than for type 2 diabetes, indicating complicated immunological pathways. Immune responses in recipients with disease-susceptible haplotypes should be monitored for several months following immunization.
Introduction
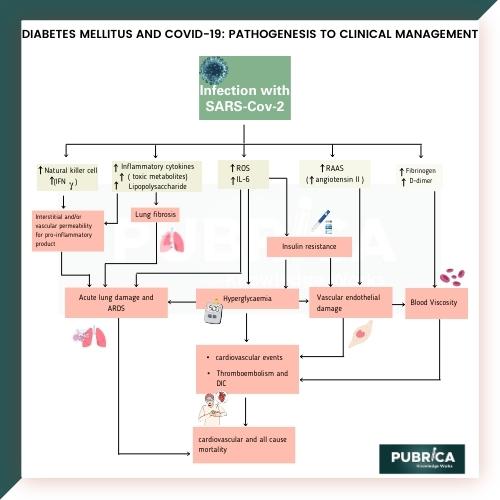
The SARS-CoV-2 outbreak has generated a cytokine storm that has affected the respiratory, digestive, circulatory, renal, and central neurological systems, resulting in organ failure. Diabetes has been associated with the virus, with consequences such as diabetic ketoacidosis and new-onset diabetes caused by altered-cell functioning. Direct SARS-CoV-2 infection causes -cell apoptosis and transdifferentiation, which is a prevalent pathophysiology in both type 1 and type 2 diabetes. The COVID-19 pandemic vaccine, which was developed to avert the pandemic, was delivered with good effectiveness and safety. The vaccination, however, has been associated with poorer glycemic control following injection.
Significance of COVID-19 vaccination for individuals with diabetes
The significance of COVID-19 vaccination for individuals with case study diabetes cannot be overstated. People with diabetes, particularly type 2, are at a higher risk of severe illness and complications if they contract the virus. Vaccination offers crucial protection by reducing the chances of infection and, more importantly, severe disease or death. It helps regulate blood glucose levels, which the virus can exacerbate. By getting vaccinated, individuals with diabetes contribute to achieving herd immunity, safeguarding themselves and others. It’s a vital step towards resuming a semblance of normalcy, easing healthcare systems, and preventing long-term health complications. COVID-19 vaccination is an essential tool in the fight against this pandemic, particularly for those with diabetes.
Case Report
A 73-year-old Japanese lady with a history of osteoporosis and non-tuberculous mycobacterial infection developed mild glucose intolerance. She matched the American Diabetes Association’s diagnostic criteria for diabetes three months before the first COVID-19 vaccine. Her HbA1c level was reduced without additional treatments. She developed fever and malaise after getting two doses of the Moderna COVID-19 vaccine, which disappeared within a few days. Her HbA1c level climbed to 7.3% four weeks after the second vaccine, and she had anorexia, exhaustion, nausea, and vomiting three weeks later.
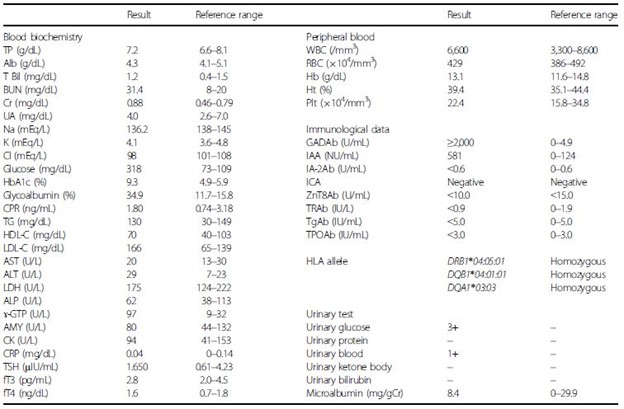
A type 1 diabetic patient’s blood glucose control deteriorated eight weeks following her second immunization. The HbA1c level was 9.3%, the casual blood glucose level was 318mg/dL, the serum C-peptide level was 1.80mg/mL, the anti-glutamic acid decarboxylase antibody level was >2,000mg/mL, and the insulin autoantibody level was 581mg/mL. The polymerase chain reaction test for COVID-19 was negative, and no infection was discovered. A dynamic computed tomography scan revealed no tumours in the liver or pancreas that might be contributing to poor glycemic control. A glucagon stimulation test revealed that the patient was insulin-dependent and was homozygous for one of the vulnerable human leukocyte antigen haplotypes for type 1 diabetes.
Table 1 Blood and urinary data of the patient (Hironobu Sasaki et al. 2022)
Management and interventions
After initiating aggressive insulin therapy, the patient’s glycemic control improved and remained stable, and all hyperglycemic symptoms vanished. There were no diabetic microvascular complications or autoimmune thyroid disorders in the patient. Fasting blood glucose and serum C-peptide levels were 89 mg/dL and 0.42 ng/mL, respectively, 12 weeks after the second immunization, indicating that the patient was still insulin-dependent. The change in HbA1c before and after the vaccination is shown in Figure 1.
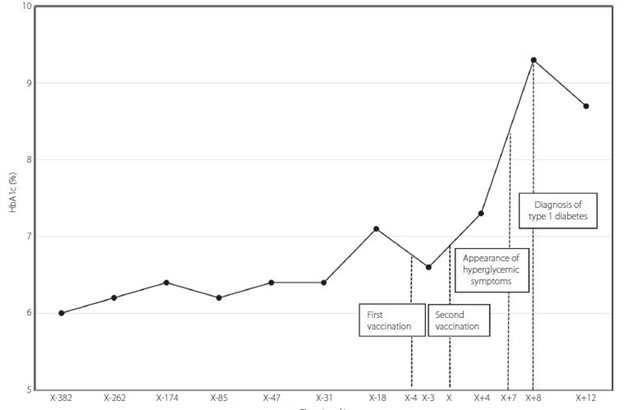
Figure 1 | Glycated haemoglobin (HbA1c) changes before/after coronavirus disease 2019 vaccine administration. The reference date of the time axis (day X) was set as the date of the second vaccination. (Hironobu Sasaki et al 2022)
Discussion
COVID-19 vaccines may cause diabetes in patients, increasing the risk of hyperglycemia. The diagnosis of type 1 diabetes took a longer period after the second vaccination, suggesting multiple mechanisms. The administration of adjuvants to genetically predisposed individuals can cause autoimmune responses, leading to the autoimmune/inflammatory syndrome induced by adjuvants (ASIA syndrome). Monitoring patients with disease-susceptible haplotypes is necessary for the elucidation of the mechanism.
To know more about research services, check our study guide on the principles of experimental design for research.
Conclusion
In conclusion, the patient, who had no episodes of infection preceding the onset of the disease and was under good glycemic control over a long period with good adherence to dietary and exercise therapy, suddenly showed hyperglycemic symptoms and a quite high HbA1c value with high titers for autoantibodies against glutamic acid decarboxylase and insulin, suggesting the development of type 1 diabetes attributable to COVID-19 vaccination. Because patients with the disease-susceptible haplotype, as in the present case study research, might need to be monitored for autoimmune responses for several months after the vaccination, accumulation and analysis of similar medical cases of diabetes associated with the vaccination and elucidation of the mechanism are warranted.
Check our Examples to get an understanding of our adaptability across case report topics and subject domains.
About Pubrica
Pubrica’s team of researchers and authors develop Scientific and medical research papers that can act as an indispensable tool to the practitioner/authors. Pubrica medical writers help you to write and edit the introduction by introducing the reader to the shortcomings or empty spaces in the identified research field. We have extensive experience in developing a detailed clinical case report that highlights the symptoms, signs, diagnosis, treatment and follow-up of an individual patient. Our experts are aware of the structure that follows the broad topic, the problem, and the background and advance to a narrow topic to state the hypothesis.
References
- Sasaki, Hironobu, et al. “Newly developed type 1 diabetes after coronavirus disease 2019 vaccination: A case report.” Journal of Diabetes Investigation 13.6 (2022): 1105-1108.
- Yano, Masahiro, et al. “New-onset type 1 diabetes after COVID-19 mRNA vaccination.” Internal Medicine 61.8 (2022): 1197-1200.
- Sakurai, Kanako, et al. “Type 1 diabetes mellitus following COVID‐19 RNA‐based vaccine.” Journal of diabetes investigation 13.7 (2022): 1290-1292.