
How Evidence Based Practice Enables Informed Healthcare Decisions
April 15, 2021
Which is appropriate to use fixed-effect or random effect statistical model while conducting meta-analyses?
April 22, 2021Brief
Technology development has made enormous changes in all sectors. Evidence-Based Practice which is a promising one followed around the globe for better treatment of patients has also grabbed the effects of technological development. Ease of accessing the information, timely interventions, reliability are the benefits made out of technology development connected EBP.
Introduction
Evidence-Based Practice ensures the connectivity between clinical expertise and research evidence. As we go into the information age of health care, digital health technologies offer important opportunities to optimize both Evidence-based delivery and clinical literature review. Despite their potential, the use of such digital technologies in Evidence-based practice and research faces major data quality, privacy, and regulatory concerns.
Health Informatics paves a better way for managing and accessing clinical data. This helps the healthcare professionals to get the related information at essential times. Internet of Things, Machine learning, Deep learning, etc., are now in the current trend for data management and this helping the daily updates on the evidence that are made out of particular case subjects. The parallel intervention of both has made tremendous changes.
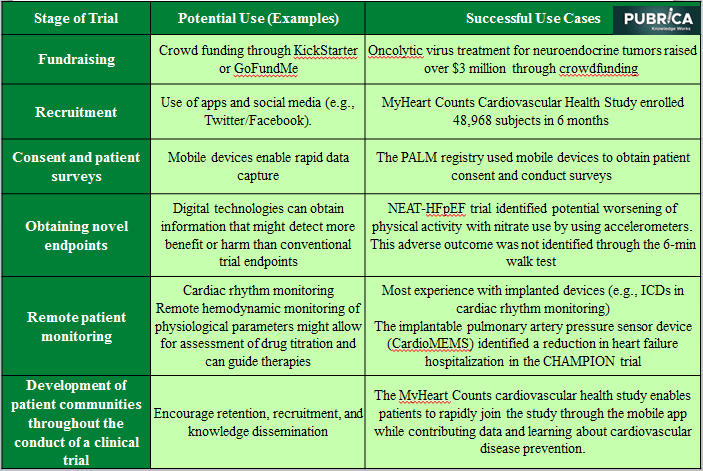
Potential Uses of Digital Health Technologies in Clinical EBP
EBP in Health Informatics
An increasing amount of clinical data and databases creates more obstacles for health professionals in reaching the appropriate information. Therefore, a need for efficient management of the information is made. Updating to the current technology becomes an essential need.
More software, toolkits, journals, research chapters, are digitalized. These are the simplest forms of technology development in the Healthcare sector. However, their more complex form of data is consolidated and made available on the Internet and in various other sources.
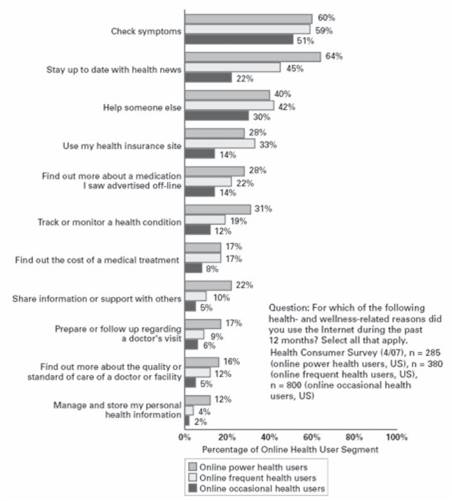
Quality of the Research Publication
There are plenty of sources available these days and the most exceptional one is the Internet where we collect more data such ah articles, review chapters, etc. But the quality of the content containing the relevant information is the most important thing to be considered before proceeding to utilize the data. The collected data must ensure validity, compliance, aftermath effects.
Merits
The data provided by professionals from anywhere in the globe can be stored and managed easily. Also, clinical data management can be improvised under an outstanding architecture and framework. The quench for necessary technology to tackle the new needs, help in the creation of new technological innovations.
To put this simple, consider the pregnancy kits; Based upon the evidence, it is known that Human Chorionic Gonadotropin (HCG) is released during the pregnancy time of women. Identifying this, to help them to detect the pregnancy, pregnancy kits were made, which is seen as an innovation in technology.
Criticisms of EBP
Though the qualitative research is the most welcomed type of research. EBP is criticized for relying more upon quantitative research. Many professionals around the globe question the definitions of the term – Evidence in Evidence-Based Practice. They argue that, based upon the perception towards the problem, the evidence can be both correct as well as incorrect. Furthermore, clinical experience is also given an equal part in creating the evidence-based medicine, thus questioning the certainty and biasness.
Conclusion
The future aspects of technology development bound with EBP are surely predictable and sound essential. There involved a lot of difficulties in experimentation, collection of data from various sources, and bringing them to the right situation at right time. Apart from all, it keeps on updating itself based on the new situations that arise after new cases.
References
- Kearsley, R., Guris, R. D., Miles, L. F., & Shelton, C. L. (2021). Case reports in the COVID‐19 pandemic: first responders to an emergency in evidence‐based medicine. Anaesthesia Reports, 9(1).
- Chandran, P. V., Khan, S., Pai, K. G., Khera, K., Devi, E. S., Athira, B., & Thunga, G. (2020). Evidence-based medicine databases: An overview. J Appl Pharm Sci, 10(7), 147-154.
- Chao, G. F., & Dimick, J. B. (2021). Evidence-Based Medicine and Decision Making. In Difficult Decisions in Bariatric Surgery (pp. 5-14). Springer, Cham.
- Liu, H., & Liu, Y. (2021). Construction of a Medical Resource Sharing Mechanism Based on Blockchain Technology: Evidence from the Medical Resource Imbalance of China. Healthcare 2021, 9, 52.
- Howell, J. D., & Long, D. E. (2019). 5. Machines and Medicine: Technology Transforms the American Hospital (pp. 109-134). Cornell University Press.
- Anjum, R. L., Copeland, S., & Rocca, E. (2020). Medical scientists and philosophers worldwide appeal to EBM to expand the notion of ‘evidence’. BMJ evidence-based medicine, 25(1), 6-8.
