
How to overcome regulatory and ethical challenges regarding medical device?
June 8, 2021
Making Sense of Effect Size in Meta-Analysis based for Medical Research
June 14, 2021Introduction
Evidence Based Practice (EBP) is the promising practice that interlinks the information collected after clinical expertise and proven research studies, so that, vital information for better healthcare management can be set and followed. The most seen purpose of EBP is assistance to clinical healthcare professionals in making decisions for better treatment of patients.
The history of EBP starts in 1970. Before the EBP, the health professionals mostly tended to rely on other experienced health professionals. Though the required information is easily accessible and based, there can be mistakes or prone to incorrect leads, pertaining to the age and memory of the health professionals. Similar to the EBP, there are Evidence Based Management, Evidence Based Medicine, Evidence Based Decision making, etc.
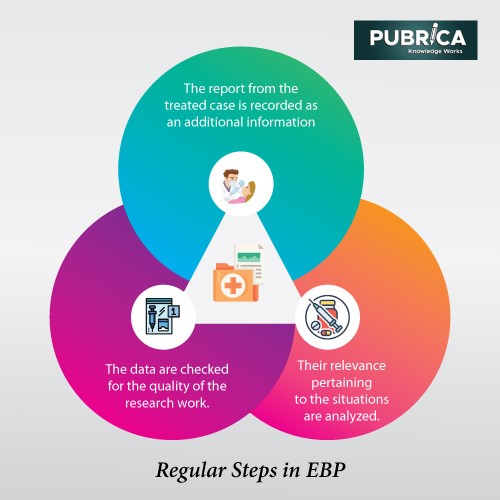
Regular steps in EBP
- Healthcare professionals cannot easily get the sources and find the necessary data. It takes more steps and time to do so.
- Firstly, based upon the patient conditions, they design a ‘need’ and start collecting the data related to that from every possible and reliable source. The data are checked for the quality of the research work.
- Later, after collecting the data, their relevance pertaining to the situations are analyzed.
- In the end, the cases are treated well and the report from the treated case is also recorded as an additional information or update of the existing information.
Medical vitality
Diagnosis is the most important step before going to treat the patient. A health professional has to hold various medical examinations and assess based upon the results. There comes a situation, where the professional has to determine the tests to be performed for the patient. Here comes, EBP in assessments and diagnosis.
Getting through uncertain medical situations, there needs an immediate measure to tackle the irregular conditions of patients. Based upon the clinical expertise alone, one cannot determine the appropriate treatment to be provided to the patient. The care plan needs to be altered according to the patients’ conditions. The handling of unexpected Covid 19 pandemic is the great example in EBP. It was a unprecedented type of disease and no researcher could able to make instant researchers upon that. All the data related to its symptoms are collected and treatment was given. Drugs used for TB and Malaria in their altered forms are used to treat the patients and recorded for future clinical research.
In this instance, let us consider the situation of a patient who met with a road accident. It is more likely to determine what exact diagnostic measures to be taken. But there can be circumstances like the patient could have had brain injury earlier. So, the patient must be diagnosed in deep for brain damage, if not that may lead to brain death.
Barriers in adopting EBP
According to the reports, a random set of nurses were asked about the barriers on their way towards adopting the EBP, in that, most of them agreed that lack of time searches for articles, at their workplace. Other reasons are– poor understandability, fear of failure, technical issues in reaching the correct resources.
EBP reports are not always completely commendable especially in the cases of severe and chronic cases. It is more important to update the knowledge not only with data based on the cases, but also through research and other studies. Sometimes, the clinical experience would even be biased based upon the varying past of the professionals.
Around the world, discussions upon EBP are yet controversial owing to the hidden fact that more of its reliability over the quantitative research. Perception of the healthcare professional varies, so the evidence. Also the bias of the professionals makes the evidence to be questioned for certainty.
Advantages & Disadvantages of EBP
EBP ensures the quality of information that is provided to the professionals. The professionals can provide the appropriate treatment and balance the other critical conditions of the patients. The decisions made on the EBP can be believed with more confidence.
Though EBP promises to be the better reliable method while comparing with others, there also exist certain disadvantages within it. EBP needs more accurate information and proven evidence which may consume more time. Considering the unexpected situations with patients, a professional may not start the Clinical research work to tackle the issues immediately.
Conclusion
Creating the evidence and connecting them to the appropriate situations is not a one-day matter. There involved a lot of difficulties in experimentation, collection of data from various sources, and bringing them to the right situation at right time. Apart from all, it keeps on updating itself based on the new situations that arise after new cases.
References
- Guyatt, G.H., Haynes, R.B., Jaeschke, R.Z., & Cook, D.J. (2000). Users’ guides to the medical literature: XXV. evidence-based medicine: principles for applying the users’ guides to patient care. JAMA, 284, 1290-1296. doi: http://dx.doi.org/10.1001/jama.284.10.1290
- B Jensen, I., BjörkBrämberg, E., Wåhlin, C., Björklund, C., Hermansson, U., LohelaKarlson, M., SchäferElinder, L., MunckAfRosenschöld, P., Nevala, T., Carter, N., Mellblom, B., &Kwak, L. (2020). Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach. International journal of environmental research and public health, 17(15), 5283. https://doi.org/10.3390/ijerph17155283.
- Hoffman, T., Bennett, S., & Del Mar, C. (2013). Evidence-based practice: across the health professions (2nd ed.). Chatswood, NSW: Elsevier.
- Hasanpoor, E., Janati, A., Arab-Zozani, M., &Haghgoshayie, E. (2018). Using the evidence-based medicine and evidence-based management to minimize overuse and maximize quality in healthcare: a hybrid perspective. BMJ Evidence-Based Medicine, bmjebm–2018–110957. doi:10.1136/bmjebm-2018-110957
