
Writing a Good Research Statement for a Faculty Position
December 5, 2022
Common Challenges for Successful Clinical Monitoring of Medical Device
December 26, 2022In brief
The miniaturization, complexity, proliferation, and accessibility of technology enable capturing inaccessible events in Parkinson’s disease (PD). However, additional information has not resulted in a better knowledge of disease complexity to meet diagnostic and therapeutic demands. Non-compatible technological platforms, the necessity for large-scale and long-term sensor technology deployment (particularly among fragile elderly patients), and the gap between “big data” obtained with sensitive measurement technologies and their restricted clinical applicability are all challenges. This blog briefly explains in early signs of Parkinson’s disease management technologies and challenges.
Introduction
Parkinson’s disease is a nervous system movement condition that leads to pain. People may experience problems with movement, tremors, weakness in the limbs or trunk of the body, or poor balance as nerve cells (neurons) in parts of the brain weaken, are weakened, or die. People may have trouble walking, talking, or completing other simple tasks as these symptoms become more noticeable. Systematic review writing services also occur in different conditions, but not everyone with one or more of these symptoms has Parkinson’s disease.
Systematic review of second most common neurodegenerative disease
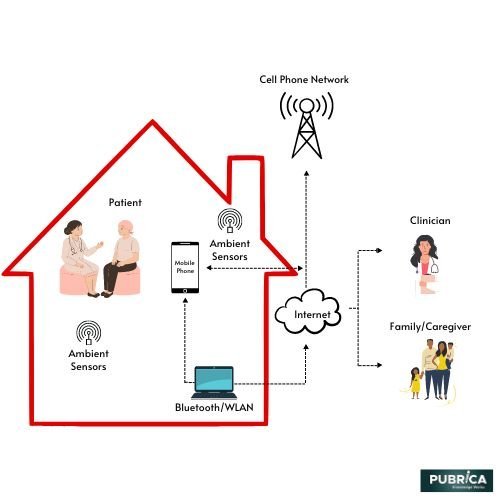
When patients with Parkinson’s disease don’t respond well to medication or their medication’s efficacy deteriorates over time, technology provides a new treatment option. Deep brain stimulation (DBS) is a well-known treatment for motor symptoms that entails the implantation of a small device that sends electrical signals to specific brain areas. This treatment will improve a patient’s quality of life by treating the disease’s motor symptoms, such as stiffness, tremor and slow movement. Rather than transmitting a constant signal predetermined by the patient’s doctor, advances in DBS technology have concentrated on making these electrical signals more resilient to fluctuations in symptoms or brain signals that the system can detect. More details about DBS’s ability to give patients better care choices that can adapt to their evolving needs will be discovered as the research of this technology progresses. Furthermore, this review directed towards the telehealth systems can assist clinicians in remotely managing patients receiving DBS at home, making healthcare more accessible to patients and demonstrating a way for clinical researchers to collect real-time data and produce endpoint data(1).
Challenges
The need for monitoring non-motor symptoms
The development of wearable systems to monitor individuals with Parkinson’s disease has been focused heavily on motor aspects of the disorder (e.g., dyskinesia, gait impairment, bradykinesia and tremor, which are also, albeit with lower specificity and sensitivity, evaluated by clinical scales. Despite recent developments in quantifying motor symptoms like tremors, these endpoints have an only minor quantitative agreement with quality-of-life indicators.
- Non-motor deficits often cause patient priorities and motivations of impairment (e.g., sleep disturbance, orthostatic hypotension, fatigue, anxiety, depression).
- Unfortunately, clinical trial systematic review services of few studies have concentrated on capturing the variations of these dynamic disease presentations, characterized by high variability within and between days.
- Labour-intensive or computerized, laboratory-based measurements have been used to establish technology-based objective measures (TOMs) for non-motor endpoints (e.g., sleep, blood pressure changes, heart-rate variability or cognitive function.
- Therefore, developing unobtrusive systems to track non-motor endpoints in the home and community is critical(2).
Limitations of sensors used to monitor motor symptoms

Magnetometers, gyroscopes and accelerometers are biomechanical sensors that detect tremors, bradykinesia, gait dysfunction, and motor problems, including dyskinesia.
- Data obtained using these sensors in the home and community does not always provide enough information to make an accurate clinical evaluation of motor symptoms.
- Determining whether slowness can be used as a proxy for bradykinesia or is the product of fatigue or other factors relevant to the context in which motor activity is performed is complicated based on sensor data alone (e.g., slow walking due to fear of falling).
- Furthermore, biomechanical sensors’ resolution is limited to the anatomical region on which they are used, resulting in poor quantitative agreement with a broader spectrum of motor dysfunction, quality of life, and other observable patient-relevant endpoints(3).
Conclusion
Despite the obstacles, continuous advancements in sensors’ technical wearability, versatility, and complexity have provided opportunities to capture disease-relevant data using patient-relevant and responsive to Parkinson’s disease-specific symptoms and milestones goals. To turn these possibilities into better treatment, better self-management choices for Parkinson’s disease patients, and overall better health care outcomes, innovations will have to be created 1) open platforms that can be incorporated with electronic medical record systems be developed, 2) integrated into treatment delivery systems and 3) suitable for capturing motor and non-motor phenomena.
About Pubrica
Pubrica’s team of researchers and authors create scientific and medical research papers that can be used by practitioners and authors as reference materials. Pubrica medical writers assist you in writing and editing the introduction by introducing the reader to the deficiencies or gaps in the identified research field. Our experts understand the structure that begins with a broad topic, progresses to a problem, and then to a narrow topic to state the hypothesis.
References
- Bayestehtashk, A., Asgari, M., Shafran, I., & McNames, J. (2015). Fully Automated Assessment of the Severity of Parkinson’s Disease from Speech. Computer Speech & Language, 29(1), 172–185. https://doi.org/10.1016/j.csl.2013.12.001
- Berganzo, K., Tijero, B., Gonzalez-Eizaguirre, A., Somme, J., Lezcano, E., Gabilondo, I., Fernandez, M., Zarranz, J. J., & Gemez-Esteban, J. C. (2016). Motor and non-motor symptoms of Parkinson’s disease and their impact on quality of life and on different clinical subgroups. Neurologia (English Edition), 31(9), 585–591. https://www.sciencedirect.com/science/article/pii/S2173580816301109
- Wicklund, E. (2021). Chicago Hospital Uses Telehealth to Manage DBS Treatment at Home. https://mhealthintelligence.com/news/chicago-hospital-uses-telehealth-to-manage-dbs-treatment-at-home
