A Systematic Review and Meta-Analysis of Plant cell technology for Production of Natural-based Drugs – Protocol and Brief Outcome – Paper Commentary.
April 13, 2022
A systematic review of quality standards for medical devices and practice measures for patient safety
April 28, 2022In brief
In new medications, the FDA’s clearance procedure is designed to provide consumers confidence that a medical device will be safe and effective in its intended use once it comes to market. The typical time it takes to get a device to market is 3 to 7 years, compared to 12 years for pharmaceuticals. However, there are concerns that the Food and Drug Administration’s Systematic Review Writing methods may not be adequate to satisfy the required guarantees of safety and efficacy. This blog aims to review the second part of a two-part series on the essential phases in medical device development and FDA clearance and summarise post-marketing protocols for pharmaceuticals and devices (J Am Coll Cardiol Basic Trans Science 1:277–87, 2016). The Authors, 2016. Elsevier represents the American College of Cardiology Foundation. The second part of a two-part series discusses the fundamental phases in medical device development and FDA clearance and the post-marketing processes for medications and devices.
Introduction
The FDA’s Center for Devices and Radiological Health (CDRH) oversees device regulation. A device is defined as “an apparatus, instrument, contrivance, implement, machine, implant, or in vitro reagent” that meets three criteria: 1) it is recognised in the official National Formulary or the United States Pharmacopeia; 2) it is intended for use in the diagnosis of disease or other conditions, or the cure, mitigation, treatment, or prevention of disease; or 3) it is intended to affect the structure or utility of the human body. Devices cannot achieve their goals by chemical action or by metabolism. Some biologically based products are inert (e.g., acellular dermatologic fillers) and classified as devices. According to the FDA, medical devices include tongue depressors, stethoscopes, lab equipment, surgical tools, and life-support equipment, including pacemakers, ventilators, and perfusion systems. If a product is a device or a biological, the FDA’s Device Determination Officer can help.
The Pre-Clinical Stages: Prototype Development and Testing
Many of the new medical gadgets on the market are adaptations of prior equipment. A physician or bioengineer’s proposal for a remedy to a medical condition is usually the starting point for developing an altogether new device. In Conducting a Systematic Review, they create or arrange to construct a preliminary prototype of the device while also starting the patent procedure. Animal testing follows initial bench testing, and the device then enters a testing and redesign cycle that takes 2 to 3 years and costs between $10 million and $20 million. Because of these expenditures, venture-backed startup firms rather than university medical institutes now produce the majority of really novel medical devices.
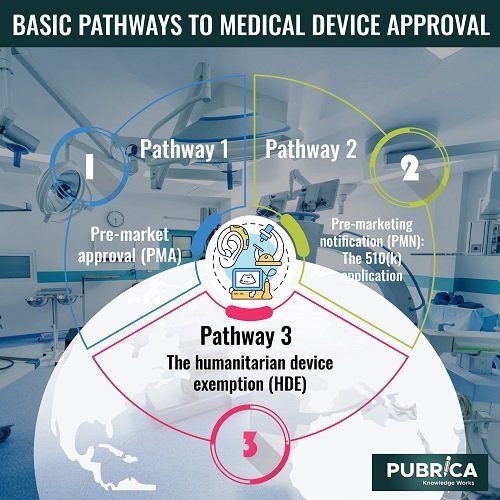
Basic Pathways to Medical Device Approval
Depending on the type of the item and the conditions under which approval is requested, there are 3 main stages for obtaining FDA marketing clearance for medical devices: Three processes are: 1) the PMA, 2) the PMN, and 3) the humanitarian device exemption (HDE).
Pathway 1: Pre-market approval (PMA)
Federal law requires device makers to inform the FDA of their intent to commercialise a medical device at least 90 days before release. The FDA requires a PMA for every new device for which there is no existing equivalent or predicate unless the device can be classed as a “de novo” device. A device must be proven to have enough scientific Systematic Review Service evidence that it is safe and effective in its intended application to receive a PMA.
Pathway 2: Pre-marketing notification (PMN): The 510(k) application
A PMN, also known as a 510(k) application, is a fast-track process for medical devices in which the sponsor demonstrates that the product is substantially identical to an authorised and marketed item. Devices under PMA evaluation but not yet authorised cannot be used as a predicate device in a PMN for a separate, new device. A PMA application is not required if the FDA decides that the device has an acceptable predicate, and PMN can proceed.
Pathway 3: The humanitarian device exemption (HDE)
A humanitarian use device (HUD) is a medical gadget designed to treat or diagnose illnesses that affect less than 4,000 people in the United States each year. The FDA’s Office of Orphan Products Development is in charge of HDE. In addition to FDA permission, the use of a HUD needs approval and monitoring by a local IRB. The application for an HDE is similar to that for a PMA, except that scientific evidence of efficacy is not required, based on the rationale that finding enough subjects to provide sufficient power for a clinical Trial Systematic Review Services to achieve statistical significance could take years.
Devices: post-market regulations and processes.
If a device fulfils any of the following requirements, the FDA may compel manufacturers to implement post-marketing surveillance programmes and submit a post-marketing surveillance report.
- Its failure would very certainly result in catastrophic health effects;
- It is predicted that it will be widely used in paediatric populations.
- It is designed to be a life-sustaining or life-supporting device used outside of a device user facility, or
- It is intended to be implanted in the body for more than one year.
Conclusion
Drug and device approval processes have a great deal in common. Each offers unique pre-submission prospects for FDA engagement. There are three basic routes to approval for each. A major road (the Investigational New Drug Application and the PMA, respectively) requires strong clinical proof of effectiveness and safety and a channel for an emergency usage (the emergency investigational new drug and the Emergency Use notification, respectively). The investigator faces a series of challenges, the first of which is to choose which path to take. Early and regular engagement with the FDA is recommended to minimise errors and difficulties that waste time and money.
About Pubrica
Pubrica’s team of researchers and authors develop Scientific and medical research papers that can be indispensable tools to the practitioner/authors. Pubrica medical writers help you write and edit the introduction by introducing the reader to the shortcomings or empty spaces in the identified research field. Our experts know the structure that follows the broad topic, the problem, and background and advance to a narrow topic to state the hypothesis.
References
- U.S. Food and Drug Administration. CFR-Code of Federal Regulations Title 21 vol. 8 Sec 870.3610 Implantable pacemaker pulse generator. Available at: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/ cfCFR/CFRSearch.cfm?fr¼870.3610. Accessed March 4, 2016.
- Van Norman, Gail A. “Drugs, devices, and the FDA: part 2: an overview of approval processes: FDA approval of medical devices.” JACC: Basic to Translational Science 1.4 (2016): 277-287.
