
Importance of meta-analysis in medical research
January 8, 2021
The benefits of R programming in clinical trial data analysis
January 19, 2021In Brief :
- Biostatistics Services is important for collecting, reviewing, presenting, and interpreting data in clinical research.
- Applications of clinical biostatistics services are in different areas, such as epidemiology, clinical trials, population genetics, the biology of structures, and more.
- It helps make decisions about the effectiveness and safety of a medication, line of care, or therapy in clinical research.
Introduction:
The global pharmaceutical industry has been facing problems in recent years, with cost inflation and drug growth delays. The twin objectives of biostatistics consulting services– saving of expense and time – have culminated in the globalization of clinical trials to developed countries. The differences between developed and developing countries in regulatory systems, ethical concerns, medical skills, clinical practice and health facilities make the third goal challenging and demanding: conformity with global quality. Globalization and outsourcing of clinical trials have completed it challenging and tough to attain global consistency.
Biostatistics Services:
Biostatistics CRO is a science branch that focuses on creating and applying statistical techniques to address health-related issues such as medicine, epidemiology, and public health.
Clinical trial quality:
Biostatistical Services offers quality that can be characterized as the absence of errors that matter in clinical trials. The prosecution’s quality essentially depends on a well-articulated forensic strategy (e.g., protocol, analysis and management plans). Clearly defined goals and related result metrics should be included in the trial.
Concept of Quality in Clinical trial:
Biostatistics for clinical research have universal ethics, and scientific professional criterion for clinical trials’ execution is Good Clinical Practice (GCP). The GCP norm extends to all facets of the clinical trial process. The standard is a spectrum under the GCP guidance, which starts with designing, is crucial during conducting and documenting, and continues during trial reporting. A lack of protocol consistency or a case record type (CRF) will also increase reporting observations and data queries. Including the notions of benefit, GCP definition of consistency has been updated: the possibility of a new medical organization (NME). Quality is defined by the Clinical Trials Transformation Initiative (CTTI) as the ability to react adequately to the expected question about the advantages and risks of a medical product (therapeutic or diagnostic) or procedure.
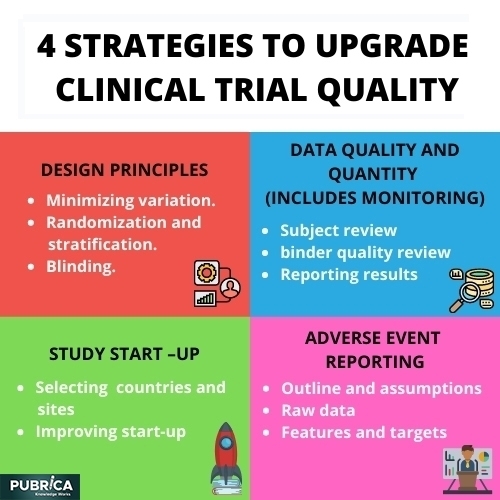
Four strategies to upgrade clinical trial quality:
The CTTI has launched several programs to identify activities that can improve clinical trials’ consistency and reliability. Statistics in clinical trials have four research focus areas: Designed principles, data quality and quantity (including monitoring), study startup and adverse event reporting.
- Design principles:
- Minimizing variation: The higher the difference, the harder it is to track medication results. Minimizing heterogeneity is, therefore, a central aspect of the nature of clinical trials. An end-point, for example, maybe the diagnosis of neuropathy or dementia. These evaluations, however, are partially arbitrary. Biostatistics consulting firms get the result with simple descriptions, and consistent assessments, heterogeneity in these diagnoses can be reduced.
- Randomization and stratification: Randomization is a powerful instrument that allows in clinical trials to control bias. It effectively removes the stigma involved with the selection of medication. Biostatistics in clinical trials equilibrium expectation given by randomization and the ITT principle provide the basis for statistical inference.
- Blinding: Blinding is an essential tool in the design of clinical trials and an effective mechanism for bias prevention and reduction. Blinding refers to holding study participants, researchers, or assessors unaware of the intervention assigned. They may be less likely to have biased psychological or physical reactions to intervention when study participants are blinded.
- Data quality and quantity (includes monitoring):
· Subject Review: The subsequent key displays, as applicable, should be revised on an ongoing foundation by an experienced person other than the person entering the information:
- Informed Consent, Assent Process
- Eligibility Criteria
- Concomitant/Prohibited Medications
- AE/SAE and UP Reporting
- Investigational Product Administration
· Binder Quality Review: A quality review of necessary forms would contain all documents registered in the International Conference on Harmonisation (ICH), and Guidelines for Good Clinical Practice (GCP).
· Reporting Results: It is essential to prepare periodically (e.g. monthly or quarterly) reports summarizing quality reviews results. The entire research team should share these reports with them.
- Study startup:
- Selecting countries and sites: As most clinical trials are global and the selection of sites is multi-factorial when discussing sites’ selection, this means the evaluation and selection process for prospective investigators’ clinical study. Of course, CROs and sponsors are looking to get the most qualified and correct sites and researchers, which generate rivalry between them.
- Improving startup: A common mistake is to rely on too little data or personal information when making decisions about a country’s involvement, sites for study conduct or recruitment strategies. It includes country and site selection based on personal preferences.
- Adverse event reporting :
Any unfavourable or unintentional symptom or indication momentarily associated with an investigational intervention during the conduct of a clinical trial, including a shift in laboratory results. Whether this incident is considered related or unrelated to this action does not matter.
- Outline and assumptions: The purpose of this attempt at proof-of-concept (PoC) was to
Develop and test a predictive model’s output that can help diagnose AE under-reporting. Here may be a fundamental link between the drug intake and the incidents reported to the sponsor in due time.
- Raw Data: To mitigate the risk of having studied with under-reporting in our data set, we used only data from completed and terminated clinical trials, where AE reconciliation had been performed as part of the study closure activities.
- Features and targets: To construct features, we needed to project all data attributes to the visit level. For demographic characteristics that were constant, such as sex and ethnicity, or had a direct dependence on the date, such as age, this was straightforward. For medical history, we counted the events that occurred before every visit.
Conclusion:
The roles and responsibilities of Statistical Programming Services are overlapping. All disciplines have distinct focuses, however. Clinical research, systematic reviews, and the working climate are complex and multidisciplinary in biostatistical activities. Therefore, biostatistics Support Service is essential for fruitful, efficient, and high-quality collaborations to clearly define the responsibilities. For which the ICH E6 guidance similarly formulates the tasks by concerning good clinical practice.
References:
- Institute of Medicine Assuring data quality and validity in clinical trials for regulatory decision making: workshop report Accessed December 21 2010
- Clinical Trials Transformation Initiative. [last accessed on 2011 May 2]. Available from: http: / /www.trialstransformation.o
- Kleppinger CF, Ball LK. Building Quality in clinical trials with the use of a quality systems approach. Clin Infect Dis. 2010;51(Suppl 1):S111–6.
- Meeker-O’Connell A. Enhancing clinical trial quality: CDER perspective. [Last accessed on 2011 May 2].
