
What are the Current Challenges in Collecting Medical Data?
November 25, 2020
Deep Learning Over Machine Learning
November 30, 2020Table of Content
In-Brief
- Precision medicine can allude to a treatment that might be individualized to a particular patient, which isn’t the genuine meaning of accuracy medicine and gives exactness medication tries to make medicines that are appropriate to gatherings of people who meet specific attributes.
- EBM has been criticized since his quality mark has been misappropriated by vested interests, the benefits statistically significant may be marginal in clinical practice, rigid rules and technology may produce care that is management driven rather than patient-centred
- Both medicines have specific advantages and limitations. Pubrica explains you the restrictions in both comparatively using Clinical biostatistics services.
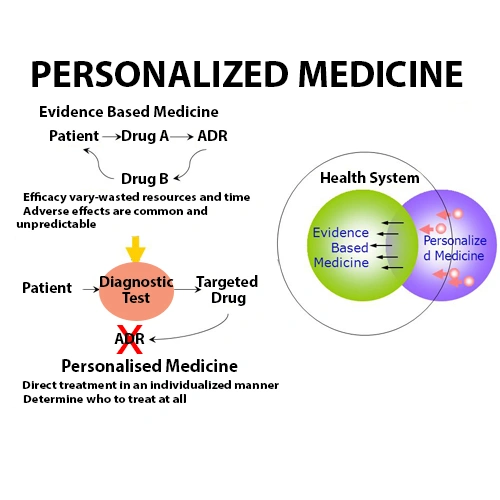
Evidence-based medicine vs precision medicine
Evidence-based medication (EBM) speaks to a worldview for clinical practice that developed out of a requirement for more apparent objectivity in clinical dynamic. EBM characterizes with “faithful, express, and prudent utilization of current best proof in settling on choices about the consideration of individual patients,” as opposed to settling on clinical choices exclusively on clinical experience and pathophysiologic rationale. EBM is presently broadly acknowledged as ideal practice for dynamic in wellbeing care using Biostatistical Services. EBM depends on three crucial standards. There is a chain of importance of proof-dependent on study plan—from approaches that are at lower danger of predisposition (for example thoroughly led randomized controlled preliminaries) to methods that are at higher threat of inclination (for example observational examinations). Second, educated clinical dynamic requires utilization of all best accessible proof, as a rule from orderly surveys to evade choice inclination. An outstanding asset is the Cochrane Collaboration, which gives audits of evidence from similar research. Third, evidence alone is never enough for clinical dynamic, and clinicians should likewise think about patient’s qualities and inclinations. The use of EBM has been appeared to bring about better results for patients. For instance, the improvement of the British Thoracic Society’s 1990 asthma rules prompted an expanded solution of breathed in steroids and utilization of individual consideration plans, and in this way encouraged diminished bleakness and mortality rates. Another model is the UK National Institute for Health and Care Excellence rules for counteraction of venous thromboembolism following a medical procedure, which prompted decreases in thromboembolic inconveniences,say biostatistics consulting firms
Limitations
Everyday impacts
While EBM gives numerous significant advantages to clinical dynamic, it isn’t without restrictions. Some have criticized EBM for zeroing in on gatherings of patients as opposed to on the individual. Specifically, when trialists report proof for treatment viability, the outcomes are frequently founded on the average treatment impact and don’t matter to all patients using Biostatistics for clinical research. Nonetheless, direction exists for revealing the extent of patients that experience significant advantage, rather than zeroing in just on expected effects.
N-of-1 Trails
Randomized controlled Trails (RCTs) from the statistics in clinical trials specific investigation configuration to set up a proof of treatment adequacy; notwithstanding, the outcomes are generalizable to patients that take after the examination populace. To keep up methodological protection against the danger of inclination in RCTs, and to guarantee relevance to singular patients, N-of-1 RCTs have been proposed for assessing treatment impacts in individuals. In such preliminaries, the exploratory mediation and control are directed two by two and requested arbitrarily to affirm the adequacy of therapy among individual patients. The number of sets of intercessions changes typically from two to seven, yet the clinician and patient can choose to stop when they build up that there are, or are not, significant contrasts between mediations
Precision medicine
Precision medication (PM), also called customized or individualized medicine, tailors the analysis and treatment of illnesses to the individual dependent on a hereditary, biomarker, phenotypic, or psychosocial attributes; as such, it is the idea of managing the correct treatment, to the valid patient, at the privilege time. The ongoing consummation of the Human Genome Project, alongside mechanical advances for describing patients utilizing proteomics, metabolomics, and genomics, gives an extraordinary and energizing open door for the PM to assume a significant function in clinical choice making. Proponents of PM propose it can re-centre medication from response to anticipation, direct the choice of ideal treatment, improve personal satisfaction, decrease antagonistic medication responses, increment treatment adherence, and generally diminish medical services costs.
Limitations
Restricted proof of clinical advantage
Even though the guarantee of PM is alluring, and unlimited usage of multiplex hotspot testing is plausible, just 13-40% of patients selected into genotype-coordinated preliminaries have given noteworthy changes, which chances to weaken of therapy effects. With this as a primary concern, the current proof proposes that the clinical advantages of biomarker-based therapy techniques might be limited. It didn’t evaluate the danger of predisposition of people preliminaries or the general nature of proof for the results they gave an account of, and couldn’t survey impacts on by and massive endurance due to deficient information biostatistics in clinical trials.
Impediments of biomarkers and sub-atomic focused on drugs
The symptomatic exactness of genetic tests is restricted, and not all genetic markers have clinical noteworthiness. For instance, accounts for cases in which ladies have gone through the pointless evacuation of their ovaries after accepting bogus positive aftereffects of genetic testing. There is a unique requirement for better biomarkers to help with the conclusion of illnesses to help control ideal treatment. Besides, regardless of whether precise hereditary tests are there, sub-atomic focused on drugs must be built up that can effectively target flagging pathways. Accessible sub-atomic focused on drugs somewhat hinder flagging pathways and might be too harmful to be in any way utilized in mix. Moreover, albeit a few medications can target flagging pathways in disease patients, malignancy cells can build up protection from them by up-controlling the path or initiation of option pathways.
Strategy difficulties and expenses
There are strategy difficulties to the broad take-up of PM, for example, the guideline of genetic tests, so that energizes advancement yet also ensures ongoing confidentiality. Health and medication administrative specialists need to set up away from for the distinguishing proof and endorsement of customized drugs and their connected symptomatic tests for clinical use. Furthermore, the expenses of creating and promoting new sub-atomic focused on drugs are high and may redirect assets from the improvement of all the more clinically significant medications. If wellbeing and administrative specialists are to support PM research, there should be autonomous assessors who routinely evaluate the money-saving advantage proportion of focused drugs.
Conclusion
While EBM and PM have their benefits and constraints, these methodologies supplement instead of contradicting each other. Pubrica conveys that the guarantee of customized quiet consideration is ground-breaking and can essentially change medical care; in any case, the more top-notch proof is expected to direct the utilization of PM to zones in which the advantages exceed the damages using Biostatistics Support Service.
References
- Beckmann, J. S., & Lew, D. (2016). Reconciling evidence-based medicine and precision medicine in the era of big data: challenges and opportunities. Genome medicine, 8(1), 134.
- Chow, N., Gallo, L., & Busse, J. W. (2018). Evidence-based medicine and precision medicine: complementary approaches to clinical decision-making. Precision Clinical Medicine, 1(2), 60-64.




